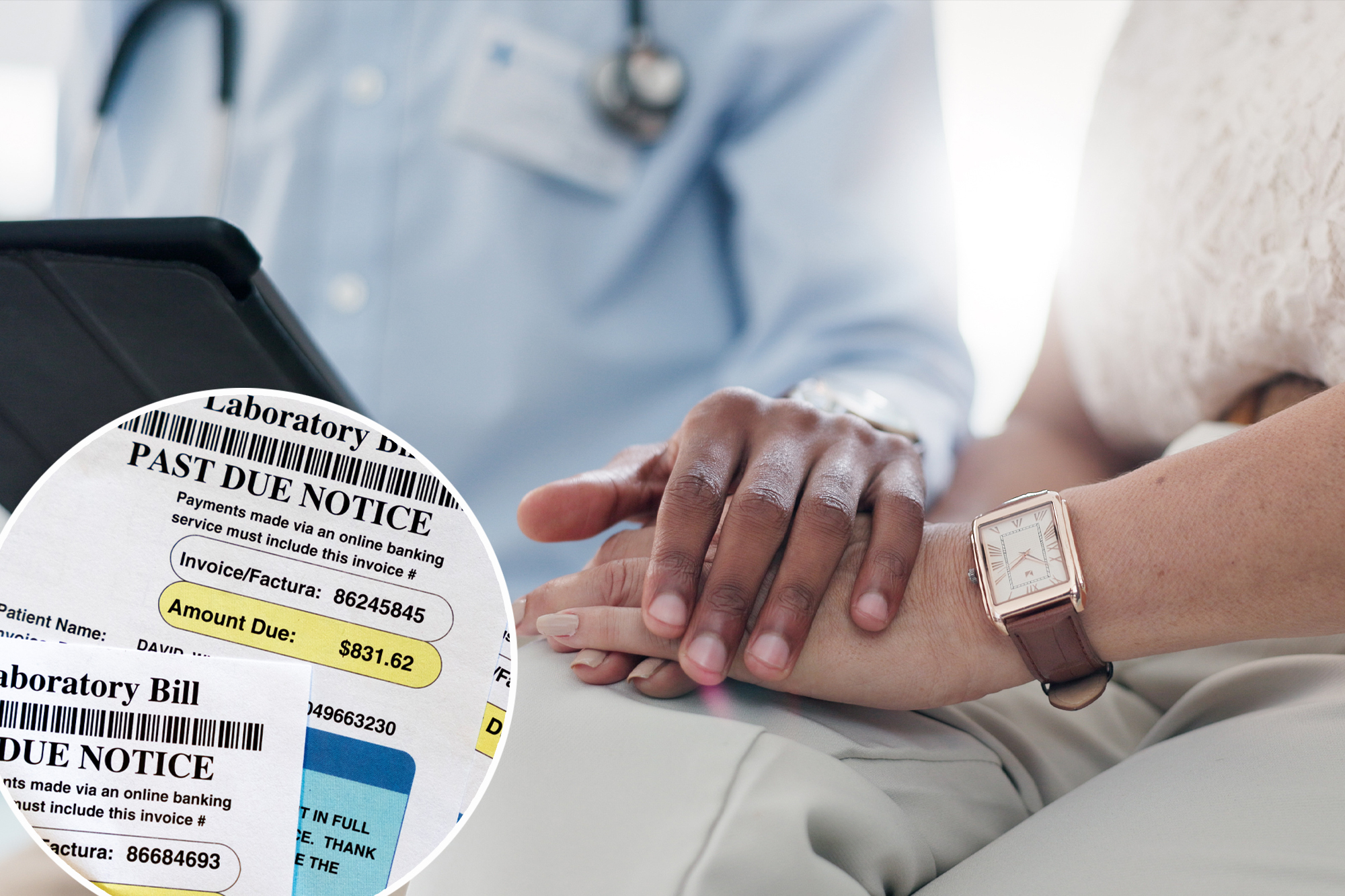
Unexpectedly high medical bills are common in the United States, but there are ways to get relief. According to the Consumer Financial Protection Bureau, one in five Americans are affected by unpaid medical debt, for a total cost of $88 billion.
In a 2022 study, the bureau found that roughly 20% of American households report having medical debt, with collections appearing on 43 million credit reports. As of the second quarter of 2021, 58% of all bills in collections on credit records were medical bills.
Medical debt also disproportionately affects families, according to the agency. Unpaid bills are more prevalent among blacks and Hispanics than whites and Asians, and medical debt is more common in the US South, in part because states in that region did not expand Medicaid coverage.
While the process of fighting high medical bills can be time-consuming and frustrating, advocates stress that patients should not be intimidated by the system. If you’ve received a surprise medical bill, here’s what you need to know:
Always check if you qualify for charity care
When Luisa, 33, received a medical bill for over $1,000 after an emergency hospital visit for a viral infection, she was able to get the entire amount covered by the hospital after turning to their financial assistance policy.
“At first I thought it was just a cold, but it turned out to be something that I needed specific medication for,” said Luisa, who asked to be identified only by her first name because of privacy concerns. “It was really bad by the time I went to the ER.”
Luisa had heard about patient advocacy organization Dollar For thanks to a viral video, and she filled out the nonprofit’s online form after receiving her surprise bill. The organization contacted the hospital, which was located in central Florida. Eventually, the hospital contacted Louise directly to let her know that she was in fact eligible for financial assistance. Although she had already paid some of the costs with a credit card, Dollar For was able to refund those payments.
Laws governing charity hospital care require nonprofit hospitals to lower or waive bills for individuals, depending on family income. To determine if you qualify, you can simply search for the hospital along with the phrase “charity care” or “financial assistance policy.” Dollar For also offers a simplified online tool for patients to see if they qualify.
“Federal law requires hospitals to have these programs to maintain their tax-exempt status,” said Jared Walker, CEO of Dollar Four. “If you’re within their income limits, they’ll write off, waive, forgive or lower your bills.”
Even if you’ve already paid off your medical debt, the hospital will be required to reimburse you for the payments you made, he said.
“It was my first time going through something like this,” Luisa said. “I tried to be an informed consumer and ask questions when I was in the hospital about costs, but obviously it’s difficult when you’re sick in the emergency room.”
Appeal to the law without surprises
While protections against unexpected bills have long existed for those with Medicare, Medicaid and Tricare, the laws are now in effect for those with private or marketplace insurance as well.
The federal No Surprises Act covers people who have insurance through their employers, the marketplace or individual plans. He says insurance companies should reasonably cover any out-of-network services related to emergency and some non-emergency medical care. This means that if you are charged more than you are used to or expect when you get services on the network, that bill may be illegal.
To challenge any bill covered by this law, you can use the Centers for Medicare and Medicaid Services’ toll-free help desk and hotline. Many states also have free consumer assistance programs to help with disputes and insurance issues.
You can always contact any hospital’s medical billing department in writing to say that you believe a bill is in violation of the No Surprises Act and request that the hospital deal directly with your insurance company.
“The complexity of the system itself is as big a problem as affordability,” said Kaye Pastaina, who directs patient advocacy research for KFF, a nonprofit health policy organization. “A lot of that comes from the fragmented system and complex rules, but also a lack of awareness of existing protections that are part of federal law that can help.”
Ask for an itemized bill
Even if you don’t qualify for charity care or aren’t sure your bills are covered by the No Surprises Act, you may be able to reduce your charges.
Medical billing is notoriously byzantine and error-ridden. Whenever you get a bill, ask the hospital or health care provider for an itemized bill that includes the billing codes for all the care you received. The Health Insurance Portability and Accountability Act (HIPAA) mandates that providers share this information.
Next, check that the billing codes are correct. Again, simply Googling the codes with the phrase “medical billing code” can help. If something isn’t right, disputing your bill with your medical provider or doctor’s office may result in changes.
Another approach: comparing the bill with the insurance company’s estimates of fair charges for services. If the price you are charged is more than the average, you can lower your costs. You can even take the provider to small claims court for non-compliance (or let them know you have a case).
Finally, compare your insurance company’s “explanation of benefits” to your bill. This explanation of covered and non-covered costs should match the hospital bill. If they don’t, you have another reason to not pay and ask the provider to work further with your insurance company first.
Remember that the process requires persistence
Despite the hassle, these steps can save you significant amounts of money. Even after taking these steps, you can always appeal health claims with your insurance company if you think there’s a reason the bills should be covered in full or more than the company initially decided.
You can also contact your state insurance commissioner for support.
“What we’ve seen in our research and the data is that those people who do appeal — and there are few who appeal — but for those who do appeal, there’s a high rate of reversal,” Pastaina said.
#relief #unexpectedly #high #medical #bills
Image Source : nypost.com